Introduction
Headaches are a common and often very painful condition, affecting a large percentage of the population. A headache is the sensation of pain in any part of the head, with the type of pain ranging from dull or aching, to very sharp in nature.
There are a wide variety of causes of headache, in fact the International Headache Society recognises more than 200 different types.(1) One of the most common varieties people suffer from is called a Cervicogenic headache, which we regularly see and treat at Spine Sport Feet clinic.
What is a Cervicogenic Headache (CGH) Understanding Cervical Spine Headaches?
A cervicogenic headache is a type of secondary headache that occurs when pain is referred from issues in the cervical spine. Unlike migraines or tension headaches, cervical spine headaches are caused by dysfunction in the neck — including the joints, discs, nerves, and surrounding muscles. This condition is sometimes described as a spinal cord headache or headache from the spine, particularly when the pain originates in the upper neck and radiates to the head.
CGH is considered a secondary headache, because it is the result of another primary condition found in the cervical spine.(2)
It is thought that about 47% of the world’s population suffer from a headache at some point, and that as many as 15-20% of that total could be cervicogenic.(3)
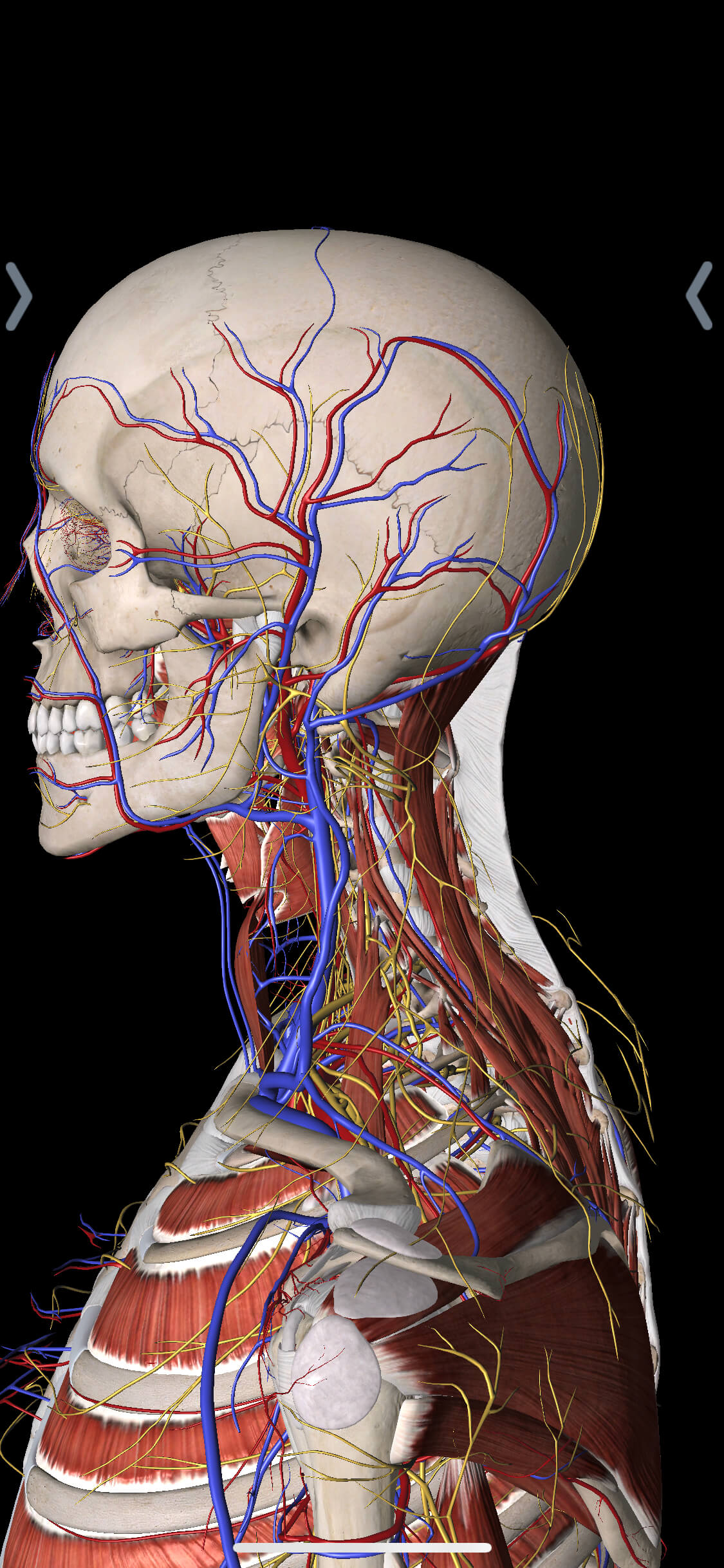
Cervical Spine Anatomy and the Trigeminocervical Nucleus
Cervicogenic headaches arise due to injury or problematic function with structures in your neck. The cervical spine contains multiple pain-sensitive structures that may trigger headaches at the base of the neck. These include cervical facet joints, spinal ligaments, vertebral arteries, and intervertebral discs. Pain signals from these structures travel through the upper cervical spinal nerves and converge in the trigeminocervical nucleus, a key area in the brainstem that also processes pain from the head and face. This explains how spinal dysfunction can result in cervicogenic headache symptoms.
Examples include:
- Cervical facet joints
- Cervical muscles
- Cervical intervertebral discs
- Facet joint capsule tissue
- Spinal ligaments
- Vertebral and internal carotid arteries
- Vertebral bone tissue
- Upper spinal cord dura mater
The above tissues send sensory information from the upper three spinal nerves in the neck to a special cluster of nerves on the lower brain stem called the Trigeminocervical nucleus. The Trigeminocervical nucleus also receives sensory information from areas in the face and head via the Trigeminal Nerve. This complex convergence of neurological feedback is what allows pain from a neck problem to be experienced in the head and face.(4)
Causes of Cervicogenic Headache and Common Risk Factors
Cervicogenic headaches can be caused by any issue creating damage and dysfunction to pain sensitive structures in the neck. They are the result of neck injury.
This can happen over a long period of time and be linked with poor work or life posture creating changes in how our head and neck are being held. This abnormal postural pattern places more stress on muscles, discs, and joints in our cervical spine.
The onset can also be traumatic such as with a fall or whiplash injury or take many years to become symptomatic as is the case with more degenerative conditions. In some cases, CGH may be due to pathology such as fractures, infection, tumours, and rheumatoid arthritis of the upper cervical spine.
The prevalence of CGH is thought to be up to 4.1% of the population and as high as 53% in headache patients following whiplash injury. The average age of sufferers is 42.9 years of age, and it is 4 more times likely to be seen in women.(5)
Cervicogenic Headache Symptoms: What to Look Out For
The Cervicogenic Headache International Study Group and International Classification of Headache Disorders have defined CGH as (5)
- One sided, non-throbbing, dull head pain with varying levels of severity and duration.
- Pain is aggravated by head movements or by long periods spent not moving the head.
- Pain radiates from the occipital region (base of the skull) to the front of the head.
- Pain may also be felt on the same side in the neck, shoulder, or arm.
- No change in symptoms with exercise, food or diet.
- No aura or pre-headache symptoms as seen with migraine.
- Aggravated by side movement and rotation of neck.
Cervicogenic headaches can be difficult to diagnose as they can mimic other conditions such as tension headaches and migraine. Many patients can in fact suffer from more than one type of headache.
Cervicogenic Headache vs Migraine: How to Tell the Difference
Cervicogenic headaches and migraines can feel similar, but they have different causes and require different treatments. A cervicogenic migraine may feel like it starts in the neck and radiates to the front of the head. However, migraines are typically associated with visual auras, nausea, and throbbing pain — features not present in a true cervicogenic headache.
If your headaches are aggravated by neck movement or posture, and don’t respond to typical migraine treatments, you may be experiencing a cervicogenic headache and migraine overlap, which can be diagnosed and treated by a chiropractor or headache specialist.
Cervicogenic Headache Treatment Options: Clinic and At-Home Care
Treatment with manual therapy such as chiropractic has shown favourable outcomes in the treatment of cervicogenic headaches, particularly when combined with exercise. (7,8) Once detailed history taking, examination, and diagnostic imaging (if required) have been performed, treatment may involve some of the following:
- Diagnosis of the primary neck issue causing CGH
- Spinal manipulation/mobilisation therapy
- Massage and muscle release
- Low Level Laser therapy
- Exercise prescription to support reduction of postural stresses
- Lifestyle, ergonomic advice
- Stretching and strengthening program.
- Multifaceted management of CGH in acute, sub-acute and chronic stages.
If you suffer from headaches or would like to know more about cervicogenic headache, please call us on (07)5580 5655 or visit our website to make an appointment with one of our chiropractors. Our practitioners use conservative, non-invasive treatment modalities and take the time to understand you. They are also well-trained to refer you to other health professionals when necessary and liaise with your doctor in such cases.
Cervicogenic Headache Treatment at Home: Self-Help Tips
While professional care is recommended for long-term relief, some people find cervicogenic headache treatment at home helpful in managing symptoms. Try the following:
- Postural correction: Avoid slouching or forward head posture at your desk or while driving.
- Heat or cold therapy: Apply a warm compress or cold pack to the base of your neck.
- Gentle stretches: Perform chin tucks, neck rotations, and shoulder rolls to reduce tension.
- Foam rolling or trigger point release: Focus on tight upper trapezius and suboccipital muscles.
Always consult a professional before starting new exercises or treatment for cervicogenic headache at home.
Frequently Asked Questions About Cervicogenic Headache
Q1: What is the best treatment for cervicogenic headache?
A: The best treatment often includes manual therapy, spinal mobilisation, posture correction, and specific exercises guided by a chiropractor or physiotherapist.
Q2: Is cervicogenic headache curable?
A: Many people experience long-term relief with proper diagnosis, consistent treatment, and lifestyle changes. While it may not be “cured” in all cases, it can often be successfully managed.
Q3: Can I treat cervicogenic headache at home?
A: Yes, stretching, heat therapy, and ergonomic changes can provide cervicogenic headache relief at home. But for ongoing or severe pain, professional care is recommended.
Q4: What causes cervicogenic headache?
A: Common causes include neck joint dysfunction, poor posture, whiplash injuries, and degenerative spinal changes — all affecting structures in the cervical spine.
Q5: Are cervicogenic headaches dangerous?
A: While not usually dangerous, they can severely impact your quality of life and may mimic more serious conditions. Proper assessment ensures the right care.
References
- www.healthdirect.gov.au : Headaches. Extracted 04/04/2022
- www.spine-health.com : What is Cervicogenic Headache? Published 12/04/2018. Extracted 04/04/2022
- Cervicogenic Headaches: An Evidence-Led Approach to Clinical Management. Phil Page, PhD, PT, ATC, CSCS, FACSM. The International Journal of Sports Physical Therapy. 2011 Sep 6(3) 254-266.
- Cervicogenic Headache: Anatomic Basis and Pathophysiologic Mechanisms. Bogduk N. Curr Pain Headache Rep. 2001 Aug; 5(4): 382-6
- www.now.aapmr.org : Cervicogenic Headache. Michael J Mehnert MD. Updated 24/07/2020. Extracted 05/04/2020
- www.spine-health.com : Treatment of Cervicogenic Headache. Zinovy Meyler, DO. Published 12/04/2018. Extracted 05/04/2020
- The Use of Manual Therapy and Exercise in the Treatment of Chronic Cervicogenic Headaches. A Series of Case Studies. Lance Whorton R, Kegerreis S. Journal of Manual and Manipulative Therapy. 2000; 8(4), 193-203
- A Randomised Controlled Trial of Exercise and Manipulative Therapy for Cervicogenic Headache. Jull G, Trott P, Potter H, Zito G, Niere K, Shirley D, et al. Spine, 2002; 27(1), 1835-1843
If you suffer from headaches or would like to know more about cervicogenic headache, please call us on (07)5580 5655 or visit our website to make an appointment with one of our chiropractors. Our practitioners use conservative, non-invasive treatment modalities and take the time to understand you. They are also well-trained to refer you to other health professionals when necessary and liaise with your doctor in such cases.